Last week we discussed a case of an immunosuppressed woman with herpes zoster infection of the face, and the concerns that go along with that (what to do with her immunosuppressive medications? Ophthalmalogic concerns? Differential diagnosis). Today, we discussed a woman visiting from sub-Saharan African with a diffuse vesicular rash, ultimately thought to be disseminated varicella with varicella pneumonia. A surprise to everyone - someone wisely ordered a BHCG and she was, in fact, pregnant.
The CDC "Pink Book" has a wealth of information on many vaccine preventable illnesses - easily found by googling "CDC Pink Book". Looking under varicella, there is access to pictures, literature, vaccine recommendations, and more. Here is the link.
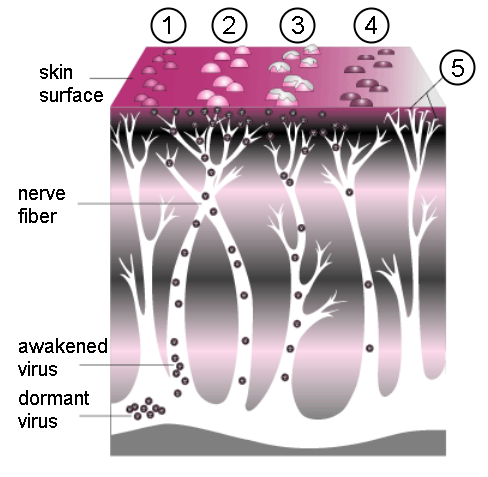
Varicella zoster virus (VZV) is a member of the herpesviridae family responsible for both acute infection ("chickenpox") and recurrent infection (herpes zoster, or "shingles"). After primary infection, VZV persists in sensory nerve ganglia and can result in recurrent infection, especially in immunocompromised hosts. It is transmitted through the respiratory tract (airborne & contact precautions in most hospitals!) with an incubation period of 14-16 days, although longer in immunocompromised hosts. Primary infection, as in our patient, is usually preceded by a 1-2 day malaise, followed by a generalized, pruritic rash that progresses from macules, to papules, to vesicular lesions, then crusts. Lesions of all ages can be found. Recurrent infection is more common in those with immunosuppression, advanced age, intrauterine VZV exposure, and VZV infection at less than 18 months. Zoster can become disseminated and involve the skin, CNS, lungs, and liver. It typically involves the fifth cranial nerve (as in our patient last week) or the trunk.
Complications can be severe, and can include:
- Secondary bacterial infection of skin lesions
- Viral or secondary bacterial pneumonia
- Meningitis or encephalitis (especially affecting cerebellum, leading to ataxia)
- Reye syndrome
- Myocarditis, GN, Transverse Myelitis, TTP, adrenal insufficiency
- Congenital Varicella Syndrome (CVS)
Congenital Varicella Syndrome is a risk if infection occurs in the first 20 weeks of gestation. Risk is actually pretty low (2%). It is manifest by:
- Low birth weight
- Hypoplasia of an extremity
- Skin scarring
- Localized muscular atrophy
- Encephalitis, cortical atrophy, chorioretinitis, and microcephaly
CVS is distinct from the risks if mum develops VZV from 5 days before to 2 days after delivery, which can result in overwhelming neonatal infection and 30% fatality rates. This is thought to be the result of fetal exposure without passive maternal antibodies.
We consider VZIg in certain populations, including:
- Immunocompromised patients
- Neonates whose mothers have signs and symptoms of varicella around the time of delivery
- Preterm infants born at or greater than 28 weeks gestation who are exposed during the neonatal period to non-immune mums
- Preterm infants born at less than 28 weeks' gestation or who weigh 1,000g or less at birth and were exposed during the neonatal period, regardless of maternal history of varicella disease or vaccination
- Pregnant women within 96 h of exposure
A few final pearls:
- All pregnant women should receive treatment (ie with acyclovir). See here for an article on management of VZV in pregnancy.
- Don't forget to consider other possibilities: Measles? Coxsackie? Impetigo? See here for some pictures and a summary table.
- Lastly, we must remember that geography plays a large role in varicella immunity. Many immigrant and refugee populations come from tropical and subtropical climates, where varicella immunity is much LOWER than in temperate climates like ours. Thus, a pregnant mum hailing from Zambia is a lot less likely than one born in Toronto to be immune to VZV. Given the risks, we should perhaps be engaging in routine antenatal screening of women from tropical/subtropical zones and providing vaccination, as well as insuring that they have access to timely and appropriate antenatal/pre/postnatal care. There has been some study on this issue, and here's an example.
No comments:
Post a Comment